EVV Aggregation Transaction Manager
Tip: You can press Ctrl-F on your keyboard to search this topic.
Access to the EVV Aggregation Transaction Manager
The HHAX EVV Aggregation Transaction Manager allows providers to manage visits (related to the linked payer placements) that have been approved or rejected by the Texas Medicaid and Healthcare Partnership (TMHP) EVV Aggregator. The TMHP EVV Aggregator is a centralized database maintained and operated by TMHP that collects, validates, and stores statewide EVV visit transaction data transmitted by the HHAeXchange system.
On the Edit Roles page (User Management > Edit Roles), Providers can assign the role permission for the EVV Aggregation Transaction Manager.
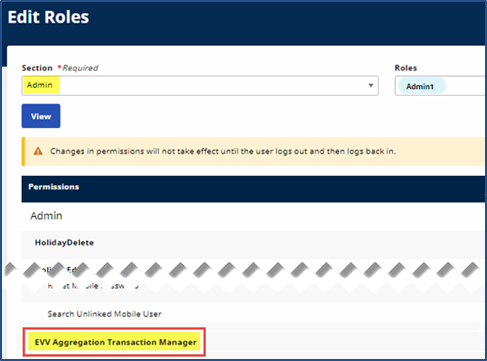
Edit Roles: EVV Aggregation Transaction Manager
EVV Aggregation Transaction Manager
Through the EVV Aggregation Transaction Manager (Admin > EVV Aggregation Transaction Manager), Providers can manage visits (related to the linked Payer placements) that have been approved or rejected by the state’s EVV Aggregator.
On the EVV Aggregation Transaction Manager page, confirmed EVV and non-EVV visits are organized onto tabs based on their Aggregation status: Ready, Hold, Sent, Approved, Rejected, and Canceled.
Status and Description for Confirmed EVV and non-EVV visits are explained in the following table.
|
Status |
Description |
|---|---|
|
All Visits |
Displays all visits at once and allows Providers to perform the corresponding action(s) for each visit in the Actions column. |
|
Ready |
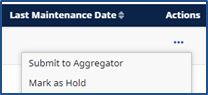
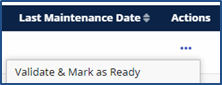
Displays all visits that are ready to be submitted to the EVV Aggregator for approval or rejection purposes. Providers can submit visits to the EVV Aggregator, mark visits as held, and cancel visits in the Actions column.
|
|
Hold |
Displays all visits that are currently on-hold due to pending reasons such as erroneous visit data, a manually performed hold, a manual visit verification, and/or an update after a visit’s Aggregator approval. Providers can validate visits and mark them as ready, and cancel visits, in the Actions column.
|
|
Sent |
Displays all visits that have been sent to the Aggregator. |
|
Approved |
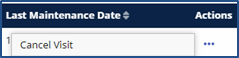
Displays all visits that have been approved by the Aggregator. Providers can cancel visits in the Actions column.
|
|
Rejected |
Displays all visits that have been rejected by the Aggregator. Providers can validate visits and mark them as ready (to reprocess through the Aggregator) and cancel visits in the Actions column. |
|
Canceled |
Displays all visits that have been canceled by the Provider. |
Resolving Held Visits in the Manager
In the Hold Status tab on the EVV Aggregation Transaction Manager page, Providers can observe the Hold Reasons and Aggregator Response to resolve the corresponding visit holds.
Hold Reasons can include standard reasons (such as Updated after Approval) or specific reasons that require correction in the Provider application, such as a Missing Medicaid ID or Missing Patient Last Name. The Aggregator Response explains to Providers the processing problems related to visits, if applicable. For example, "Patient on the EVV visit is not authorized for the Provider Number on this visit date in our records."
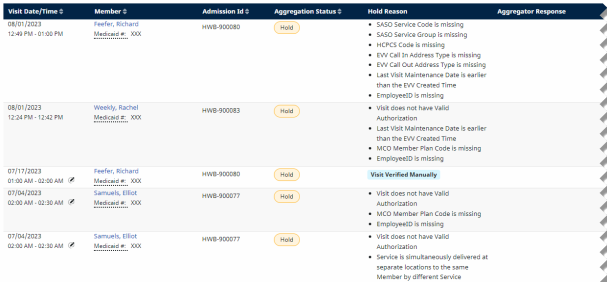
Hold Visits: Hold Reasons
The common Hold Reasons shown in the image above are described in the following table.
For a full list and descriptions of all Hold Reasons and their resolutions, see EVV Aggregation Transaction Manager Rule Holds and Resolutions.
|
Hold Reasons |
Description |
|---|---|
|
Updated after Approval |
The held visit has been approved by the Aggregator but has been newly updated. Providers can validate the visit and mark it as ready for processing. |
|
Manual Hold |
The visit has been held manually by the Provider. Providers can validate the visit and mark it as ready for processing. |
|
Visit Verified Manually |
The visit has been verified or confirmed manually by the Provider. Providers can validate the visit and mark it as ready for processing. |
|
Specific Reasons (e.g., Missing Medicaid ID) |
The visit requires corrections for problematic or missing data, such as a Missing Medicaid ID or Missing Patient Last Name. Providers can resolve such issues in the Provider application before validation processing. |