Viewing Claims Status
Payers can view a claim status any time after a Provider submits an EDI 837 Healthcare Claim to the Payer. By viewing the claim status, users can address issues before they receive an EDI 835 Healthcare Claim Remittance Advice to reduce duplicate billing.
Claims Status is displayed on the Member Calendar page (Member, Search, find and select Member, Calendar) and on the Member Visit page (Member, Search, find and select Member, Visits).
The Claim Status column is highlighted in the following image of the Member Visits page. After a visit is submitted, the Claim Status appears as a link the user can click to see Claim Details.
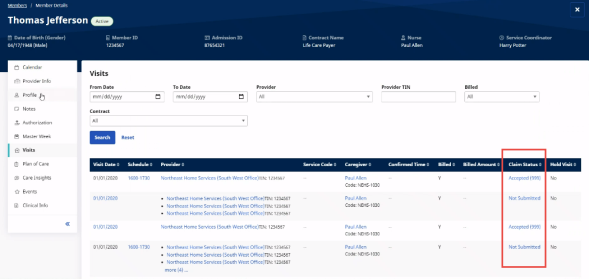
Member Visits Page: Claim Status Column
Claim Status is also displayed on the Member Calendar page, as shown below.
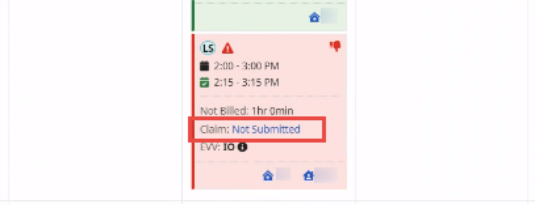
Member Calendar Page: Claim Status
Claim Status descriptions are listed in the following table.
| Status | Description |
|---|---|
| Submitted | File successfully sent from HHAeXchange, pending 999. |
| Not Submitted |
Claim waiting to be processed via the nightly process, or a technical issue occurred with the submission of this claim. |
| Unexported |
Claim being prepared for resubmission. |
| Resubmission |
Claim reprocessed and resubmitted. |
| 999 Accepted |
837 accepted by the Payer’s processing system. |
| 999 Rejected | 837 contains formatting issues due to missing information on the Member or Provider Profile. |
| 277ca Accepted | Claim accepted for processing in the Payer’s processing system. |
| 277ca Rejected |
Claim not accepted due to missing information or Member eligibility. |
Rejected Claims
The HHAeXchange Revenue Cycle Operations (RCO) Team monitors claims for rejections and attempts to resolve such issues with Providers. If a claim requires escalation to the RCO Team, submit a service ticket via the HHAX Client Support Portal and include the following information:
-
Affected Dates of Service
-
Affected Members
-
Affected Invoice or Batch Numbers
Include EDI 835 and Batch Response Files in Claim Status Info
 Setup of this feature starts with HHAX. Contact the HHAX Support Team for assistance.
Setup of this feature starts with HHAX. Contact the HHAX Support Team for assistance.
The information displayed when clicking Claim status can include a Response File History of EDI 835 Healthcare Claim Remittance Advices (835) and EDI Batch Response Files (BRF).
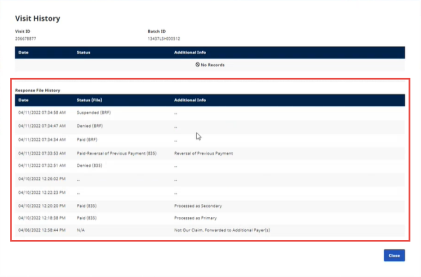
Response File History
The EDI Batch Response File (BRF) format is proprietary to the State/Payer sharing the Remittance and Claim Status information. Contact HHAX Support for assistance if a Payer wants to use the BRF format.